Abstract
Introduction
Smoldering multiple myeloma (SMM) is an asymptomatic precursor stage to active multiple myeloma (MM), comprised by a heterogenous group of patients with varying rates of progression. While the overall yearly progression rate is 10% the first 5 years, some patients progress at a considerably higher rate. A study from the Mayo Clinic showed that in a subset of 21 patients defined by ≥60% monoclonal bone marrow plasma cells (BMPC), 95% progressed within 2 years. It was subsequently concluded by the International Myeloma Working Group (IMWG) that patients with biomarkers predictive of a 2-year progression rate at 80%, and a median time to progression at 12 months were at ultra-high risk of progression and should be considered to have MM requiring treatment despite being asymptomatic. In 2014, ultra-high risk biomarkers were incorporated in the definition of MM, including BMPC ≥60%, free light chain (FLC) ratio ≥100 and ≥2 focal lesions on magnetic resonance imaging (MRI). While the updated myeloma definition changed the diagnosis of some patients with ultra-high risk SMM to MM, there remain patients classified as SMM progressing at a very high rate. In the present study, we aimed at further identifying ultra-high risk biomarkers predictive of a high rate of progression to active MM.
Methods
Patients with SMM presenting to Memorial Sloan Kettering Cancer Center between the years 2000 and 2017 were identified and included in the study. Diagnosis of SMM and progression to MM requiring therapy was defined according to the IMWG criteria at the time of diagnosis. Baseline patient and disease characteristics were collected at date of diagnosis with SMM, including pathology reports, laboratory results and imaging data. Time to progression (TTP) was assessed using the Kaplan-Meier method with log-rank test for comparisons. Optimal cut-off values for continuous variables were assessed with receiver operating characteristics (ROC) curve. Patients who had not progressed by the end of study or were lost to follow up were censored at the date of last visit. Univariate Cox regression was used to estimate risk factors for TTP with hazard ratios (HR) and 95% confidence intervals (CI). Significant univariate risk factors were selected for multivariate Cox regression.
Results
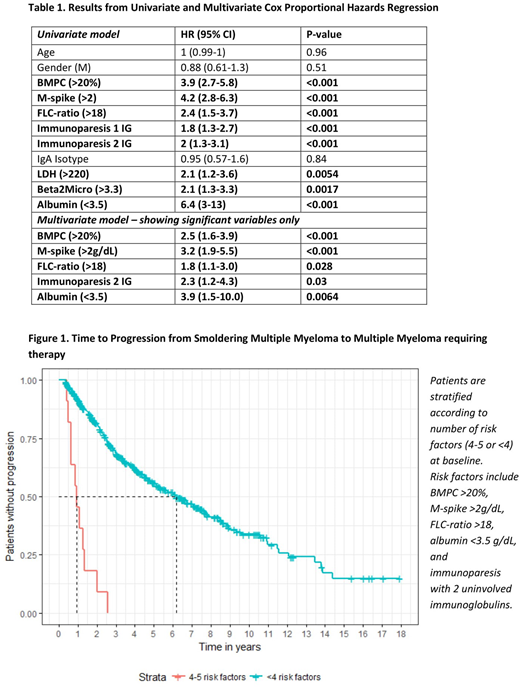
A total of 444 patients were included in the study. Median follow-up time was 78 months. During the study period, 215 (48%) patients progressed to active MM, with a median TTP of 72 months. Cut-off points for BMPC, M-spike, and FLC ratio were determined with ROC curves to be 20%, 2 g/dL, and 18, respectively, for predicting high risk of progression. The following factors were associated with significantly increased risk of progression to active MM: BMPC >20%, M-spike >2g/dL, FLC ratio >18, immunoparesis with depression of 1 and 2 uninvolved immunoglobulins respectively, elevated lactate dehydrogenase, elevated beta-2-microglobulin, and low albumin (Table 1). In the multivariate model, BMPC >20% (HR 2.5, 95% CI 1.6-3.9), M-spike >2g/dL (HR 3.2, CI 1.9-5.5), FLC ratio >18 (HR 1.8, CI 1.1-3.0), albumin <3.5 g/dL (HR 3.9, CI 1.5-10.0), and immunoparesis with 2 uninvolved immunoglobulins (HR 2.3, CI 1.2-4.3), predicted a decreased TTP (Table 1).
A total of 12 patients had 4 or 5 of the risk factors from the multivariate model, 8 of these did not meet the 2014 IMWG criteria for MM. These patients had a significantly shorter TTP than patients with less than 4 risk factors (median TTP 11 vs 74 months, p<0.0001, Figure 1). At 16 months, 82% of these patients had progressed, and within 2 years, 91% of the patients progressed. Only one patient remained progression free after 2 years, progressing at 31 months. Of patients with less than 4 risk factors, 19% progressed within the first 2 years.
Conclusion
In addition to baseline BMPC >20%, M-spike >2g/dL, FLC-ratio >18, we found that albumin <3.5g/dL and immunoparesis of both uninvolved immunoglobulins at the time of diagnosis with SMM were highly predictive of a decreased TTP to MM requiring therapy. These biomarkers are readily available and routinely assessed in clinic. Patients with 4 or 5 of these risk factors represent a new ultra-high risk group that progress to active disease within 2 years, further expanding on the definition of ultra-high risk SMM. In accordance with the rationale on ultra-high risk biomarkers as criteria established by the IMWG in 2014, such patients should be considered to have MM requiring therapy.
Korde:Amgen: Research Funding. Mailankody:Janssen: Research Funding; Takeda: Research Funding; Juno: Research Funding; Physician Education Resource: Honoraria. Lesokhin:Squibb: Consultancy, Honoraria; Serametrix, inc.: Patents & Royalties: Royalties; Takeda: Consultancy, Honoraria; Genentech: Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria, Research Funding; Janssen: Research Funding. Hassoun:Oncopeptides AB: Research Funding. Smith:Celgene: Consultancy, Patents & Royalties: CAR T cell therapies for MM, Research Funding. Shah:Amgen: Research Funding; Janssen: Research Funding. Mezzi:Amgen: Employment, Equity Ownership. Khurana:Amgen: Employment, Equity Ownership. Braunlin:Amgen: Employment. Werther:Amgen: Employment, Equity Ownership. Landgren:Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Karyopharm: Consultancy; Merck: Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Research Funding; Pfizer: Consultancy; Celgene: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal